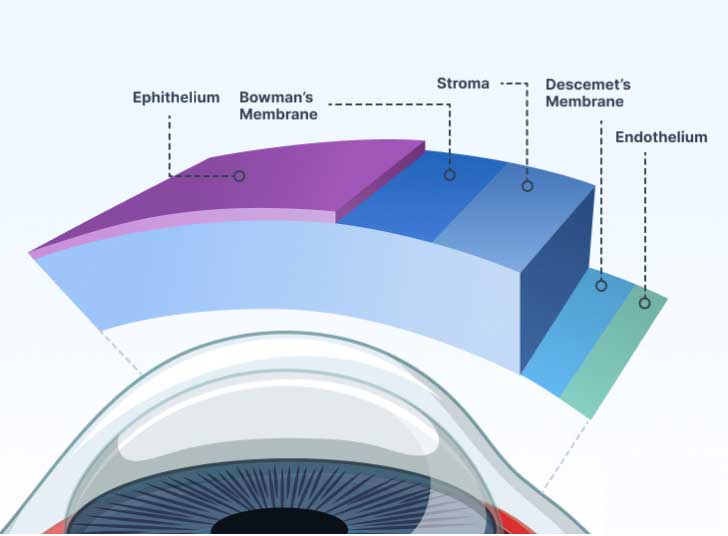
Your cornea must be clear, smooth, and healthy for good vision. If it is scarred, swollen, or damaged, light is not focused properly into the eye. As a result, your vision is blurry or you see glare.
If your cornea cannot be healed or repaired, your ophthalmologist may recommend a corneal transplant.
There are different types of corneal transplants. In some cases, only the front and middle layers of the cornea are replaced. In others, only the inner layer is removed. Sometimes, the entire cornea needs to be replaced.
Eye disease and injuries can damage the cornea. Here are some common eye problems that can lead to a damaged cornea:
If all layers of the cornea are damaged, the entire cornea may be replaced. This procedure is called penetrating keratoplasty (PK). The damaged cornea is removed and a donor cornea is stitched into place. Recovery can take a year or longer, and the risk of rejection is slightly higher than with other procedures.
With a PK, there is a slightly higher risk than with other types of corneal transplants that the cornea will be rejected. This is when the body’s immune system attacks the new cornea tissue. Click to Watch Video
If only the front layers of the cornea are damaged, those layers can be replaced while the inner layer remains intact. This procedure, called deep anterior lamellar keratoplasty (DALK), is commonly used for keratoconus. Healing is faster than with full-thickness transplants, and the risk of rejection is lower.
When the innermost layer of the cornea (the endothelium) is damaged, treatment may focus only on this layer.
Your eye surgeon will recommend the most appropriate procedure based on your corneal condition and healing potential.
Rejection occurs when the body’s immune system attacks the transplanted tissue. It is more common with full-thickness transplants and less common with partial procedures. Early treatment can sometimes reverse rejection.
Warning signs of rejection include:
Contact your ophthalmologist right away if you notice these symptoms.
If you have a damaged or diseased cornea, you and your ophthalmologist will review your options. For many patients, corneal transplant surgery can restore clearer vision and improve quality of life.